




Chronic prostatitis is a nonbacterial inflammatory condition of the male pelvis and can be considered male intersitial cystitis It is a member of the IC bladder pain syndrome(interstitial cystitis, vulvodynia, irritable bowel syndrome, GERD, and fibromyalgia) because the cause is the same as its other members Imbalances of qualities in the bowel caused by primarily the foods consumed and lifestyle choices that provoke the energy physiology lead to dissemination to the peripheral tissues Like IC itself invariably the pelvic nerves become involved with the qualities of light mobile dry rough and hot leading to observed symptoms
The presence of fever is a key differentiating feature between acute and chronic prostatitis This is very important because the treatment of acute prostatitis is completely different If a man has chills and fever of 100.5F or greater with symptoms of acute prostatitis then he should be on antibiotics and in severe cases hospitalized because the cause is bacterial
It is estimated that greater than 90% of those with chronic prostatitis are of nonbacterial origin, that is, there is no bacteria or infection in the prostate tissue Sounds a lot like IC doesn’t it?
Chronic prostatitis is not associated with fever and similar to interstitial cystitis occurs acutely as flares lasting 2-3 weeks Urological workups including cultures, xrays, and endoscopy are negative In uncommon situations cystoscopy may show bladder mucosal lesions that biopsy negative and are typically not characteristic of Hunner’s ulcers(which are unusual even in IC) Prostatic calculi may produce a chronic bacterial prostatitis but this is unusual There is no association between chronic prostatitis and prostate cancer epidemiologically in the allopathic literature
There is no agreed upon best treatment from the molecular or allopathic model of healing but it is typically treated with antibiotics initially These courses usually last for 3-4weeks or more based on the resolution of symptoms and/or recurrence of symptoms This is often the case since the cause is nonbacterial As the chronicity develops in the clinical course men are often kept on antiinflammatories or even short courses of steroids have been used
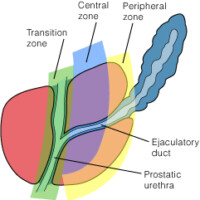
Anatomically the prostate lives at the base of the bladder and as you can see by the accompanying picture the urethral tube passes from the bladder to the outside through the penis So the symptoms of prostatitis mirror those seen in women with interstitial cystitis Suprapubic pain, perirectal or perianal pain , low back pain, testicular pain, pain referred to the base or the tip of the penis, pain with ejaculation, urinary frequency, urgency, small volumes of urine passed, and a feeling of incomplete emptying predominate when the man is having an acute flare
Due to the hot quality inflammation like IC produces the symptoms of burning on urination and because the prostate is innervated by the same use nerves affecting bladder function there can be pain with ejaculation This latter symptom may also be caused by the prostate itself becoming involved by the hot quality Sometimes the prostate becomes so inflamed that blood may be seen at the tip of the penis at the end of urination
As in IC there should be a division in treatment based on whether one is treating an acute flare or trying to do maintenance therapy This has been covered in a previous blog post Here are some basic foundational things to do
1 As always use a nutritional format appropriate for one’s energy pattern and avoid incompatible food combinations
2 Consistent daily pranayama practice specifically using kapalabhati can have symptom controlling benefit It has been shown in an Italian study of 231 sedentary men with chronic prostatitis that routine exercise helped symptoms Pranayama is an excellent combined aerobic and anaerobic exercise that stresses the pelvic floor hence strengthening this area of the anatomy which is involved in chronic prostatitis
3 Herbal formulas can be helpful even in the acute stage or flare and gokshuradhi guggulu can be effective in reducing congestion when the gland is involved
4 Basti therapy in both acute and chronic phases can be very helpful in treating the pelvic nerve imblances
5 Lidocaine as in interstitial cystitis transrectally can be helpful in reducing the acute symptoms of chronic prostatitis
Like the IC bladder pain syndrome chronic prostatitis can be healed from an energy science perspective but it requires a disciplined approach and based on how long symptoms have been present determines the length of time of recovery
Get every new post delivered to your Inbox
Join other followers
Leave a Reply